
No, we are not here to talk about a movie. But honestly, isn’t this the kind of question a patient comes with when visiting a genetic counselor? Well, at least in most cases, yes!!
Now, Imagine the intensity of this question in case of WGS and WES, where Secondary/Incidental findings are behind this DOOR.
Know The Basics
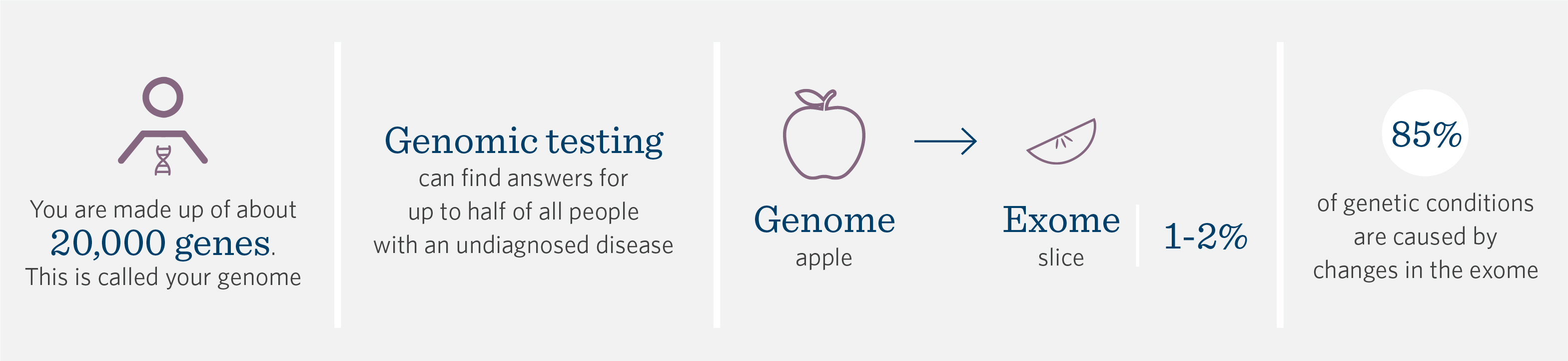
Patients and families can have varied responses to receiving genomic testing results, specially in case of WGS or WES whether positive, negative, uncertain or unexpected.

Collaboration in patient management between the referring provider and genetic counselor will lead to optimum patient care. The genetic counselor typically provides support and guidance in developing a management plan based on results. Even before we get to this management stage, what are these different results:
Positive result: A mutation was found that is known to be associated with your medical concerns. The response to this result can often be complex as some families may experience stigma or shame surrounding the fact of genetic or congenital disease or linked findings. Inherited conditions impact the whole family and result in feelings of parental guilt. On other hand, many families that undergo testing have already been through exhaustive journey of search for diagnosis and finding a pathogenic variant may provide relief and an end to long diagnosis odyssey.
Negative Result: Contradictory to above, receiving a negative result meaning no casual variant is identified, the patient and family can be feeling a sense of disappointment or a lack of diagnosis feeling as they had already made a strong mindset expecting or suspecting a syndrome. Here, it is the role of Genetic counselor to provide management plan based on clinical presentation and family history, discuss further testing if needed now or in future and mainly provide counseling to help patient/family cope with these feelings of lack of diagnosis and address psychological concerns.
VUS Results: Variants of Uncertain significance(VUS) may be reported in many tests and can be likely many in tests such as multi-gene panel, exome and WGS. Patient reactions can be very similar to that of negative results and involves regular follow up on VUS classification with the genetic provider.
Of all the above, today’s major highlight is on SECONDARY FINDINGS: The findings you weren’t looking for!!
When Exome sequencing is done, there is an option to learn about other genetic mutations. these are mutations that are not related to your primary reason of diagnosis. If these other mutations are found, these are then called secondary findings. These secondary findings although unrelated to primary reason for testing, yet can be a cause for some serious disease or heart condition which can lead to sudden death. Secondary finding can also recognize mutations which might show that patient might be risk at severe response to certain type of medications. Paradoxically, while these variants are ubiquitous in the genome, their presence must be actively sought from among the vast number of other genomic variants in order to be identifiable and reportable.
Impact of such diagnosis:
Whether a diagnosis was desired or unexpected, coming to such diagnosis often raises additional questions for the family around medical arrangement, life expectancy and social issues. There may also be healthy or reproductive risks for family members such as siblings.
Role of Genetic counseling in this aspect:

Genetic Counselling as we all know is a profession focused around the central element of non- directive approach and “patient choice.” This element plays a key role in the process of addressing secondary findings. There is a huge room for flexibility in approach and workflow to follow in genetic counseling setups and the common view from many research studies have suggested that dealing with secondary findings and whether to get secondary findings, whether to disclose or not; all these aspects lie inside the circle of the patient case you are dealing with, pre-counseling and setting expectations, providing clear information on test options, what these tests can mean to the patient and their family, their rights to informed consent and choice to not know these results and alternatives.
An example of one such workflow:

Tips for supporting families with genomic test results:
- Being aware of factors that can influence understanding of or coping with results:
a. Potential emotional reactions to results
b. Existing experiences and underlying pyschosocial issues
c. Health Literacy level and baseline understanding of genomic testing
2. Elicit knowledge and validate unique feelings that arise from genomic results.
3. Think ahead about the kinds of pyschosocial referrals that might be appropriate and have support resources specific to diagnosis available to provide.
4. Create a plan for next steps with family, specific to their results.
Recommendations by many different boards of Genetic Counseling:
- Include awareness of results to expect in pre-test counseling and informed consent discussion.
- Make them aware of their rights and choice to receive or not receive such variant or secondary findings results and what could be the implications of their choice and the results itself. That being said, enabling a patient to make an informed decision remains the responsibility of the clinical provider, a role that has not changed with the expansion of testing from single gene tests to whole-genome sequencing.
- The responsibility as to how, when, and, if results should be communicated is on a medical professional’s judgment. This patient-centric approach demands a robust informed consent process prior to clinical sequencing. It prompts questions of which information should be included and how it should be tailored to promote patient understanding.
- Ongoing Follow- up: Regardless of result, the genetic counselor may recommend follow up with patient every 1-2 year.
- Provide References to external support or to a clinical specialist and other support groups to help deal with psychological feelings.
Conclusion:
Finding the balance between the appropriate degree of professional guidance and individual choice will require more than vigorous commentary and the reporting of subjective data on hypothetical preferences, but will require empiric data on actual decisions and their outcomes. There is a growing need to evolve and advance the traditional models of informed consent and disclosure. There is also a demanding need to develop educational strategies to enhance the way people make informed decisions that streamline, yet complement, the genetic counseling process. The most crucial aspect though still relies on interpersonal dialog of a genetic counselor to help people understand and reach complex decisions and information into a healthier choice for their individual self and family life. Educational strategies that touch both the cognitive and the emotional chords in the decision-making process by helping patients forecast their short- and long-term emotional responses to their decisions will help keep genetic counseling relevant regardless of what genomic testing looks like in the future.
Interesting videos and resources for further reference:
- Whole Exome Sequencing Secondary Findings : https://youtu.be/S_UBRcAXTf8
- Possible Exome Sequencing Test Results: http://www.learninggenetics.org/possible-results.html
- Pros and Cons of Secondary Findings: http://www.learninggenetics.org/possible-results.html
- Diagnostic uncertainties, ethical tensions, and accounts of role responsibilities in genetic counseling communication: https://onlinelibrary.wiley.com/doi/full/10.1002/jgc4.1282
- Genetic Counseling in the Era of Genomics: What’s all the Fuss about?: https://link.springer.com/article/10.1007/s10897-018-0216-x
- Disclosing Secondary Findings from Pediatric Sequencing to Families: Considering the “Benefit to Families”: https://pubmed.ncbi.nlm.nih.gov/26479565/
- Criteria for reporting incidental findings in clinical exome sequencing – a focus group study on professional practices and perspectives in Belgian genetic centres: https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-019-0561-0
- Incidental Findings with Genomic Testing: Implications for Genetic Counseling Practice: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4633435/

great article! very educative and informative.
LikeLike